Healing Horses with Regenerative Medicine
By Dr. James Bryant, DVM, Diplomate ACVS
Over the last several years, horse owners have been exposed to many new treatment options for soft-tissue and joint injuries in their horses – along with the often-confusing terminology that accompanies these new therapies: Stem cells, platelet-rich plasma (PRP) and IRAP (interleukin-1 receptor antagonist protein). These treatments plus others fall under the umbrella of regenerative medicine.
Equine veterinarians, including the doctors at Pilchuck Veterinary Hospital, have used regenerative therapies for several years now to treat horses suffering from a number of conditions, including soft-tissue injuries and arthritis. The power of regenerative medicine is that it can give horses a second chance after an injury, many times aiding in the quality of the healing and decreasing risk of recurrence.
Regenerative medicine involves using the body’s own cells to repair or replace damaged tissues. Goals include: healing the damaged tissue in an “organized” manner, ideally without scarring; preserving function; and approximating what the original tissue was like (e.g., same strength and elasticity). If healing doesn’t occur in an organized way, the new tissue won’t be as strong or resilient as the original, making the horse vulnerable to re-injury or failure in repair of the damaged tissue.
Stem cell therapy
Stem cell therapy has been used successfully to treat equine injuries involving tendons, ligaments and joints. Because embryonic stem cells (which come from a fetus or placental membrane) are difficult to obtain due to medical and ethical reasons, veterinarians began to use bone marrow as a source for undifferentiated cells. These cells are capable of maturing into a variety of cell types once out of the marrow space and under the influence of the local tissue environment, just like embryonic stem cells.
In the horse, we have two viable sites for harvesting cells: fat from the tail head region and directly from the bone marrow. In both cases, samples of cells are collected and sent to a laboratory where the cells are cultured to produce a large number of viable cells. The cells are then returned frozen on ice and can be implanted.
Another process involves concentrating the cell aspirates from either the bone marrow or fat. Cells from either location are harvested, then concentrated with a special centrifuge and injected directly into the site of injury.
The decision to use fat-derived cells, bone marrow cultured stem cells, or bone marrow aspirate concentrate is often based on clinician preference, the type of injury and the timing of when you want the cells in place. Pilchuck Veterinary Hospital clinicians tend to use bone marrow-derived techniques.


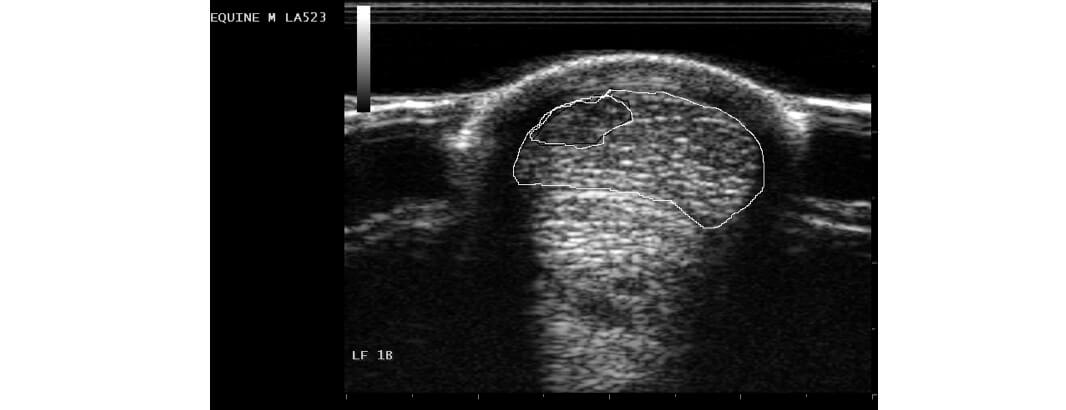
In tendon or ligament injuries, veterinarians are applying regenerative medicine therapies to horses with chronic injuries (especially in the suspensory ligament) and in acute core lesion injuries of the flexor tendons and suspensory ligament. The goal is to create an enhanced environment for healing and to provide cells that can form better collagen, which improves tendon or ligament fiber alignment. With improved healing, the likelihood of injury recurrence is decreased. An additional application of stem cells is in the joints of horses. Recent studies suggest an improved outcome in horses with soft-tissue injuries (specifically meniscal ligament) in the stifle joint.
PRP
The use of platelet-rich plasma for treating soft-tissue tendon and ligament injuries is rapidly expanding, and is sometimes used in combination with stem cell therapy. The smallest blood cells, platelets are responsible for clotting and are the “first responders” to an injury. PRP therapy works by delivering a high concentration of platelets to the injured site, increasing the amount of growth factors and helping the injury to heal. PRP is created by spinning the horse’s whole blood in a high-speed centrifuge, eliminating the red and white blood cells and leaving a high concentration of platelets in the serum. The veterinarian then injects the plasma directly into the lesion to aid in healing. Recently applications in the joint are also being used.
IRAP
Technically, IRAP (or interleukin-1 receptor antagonist protein) isn’t a regenerative therapy, but is often grouped with stem cell and PRP treatments.
IRAP therapy works by blocking interleukin-1, which causes inflammation and is naturally released from the body after an injury. Veterinarians collect blood from the horse and incubate it in the presence of chromium-coated beads, which amplify IRAP production.
IRAP is most commonly used as a joint therapy in horses for the treatment of synovitis and early arthritis. Post-joint surgery patients are also excellent candidates for IRAP. IRAP is especially exciting due to its potential for addressing osteoarthritis, one of the main causes of lameness in horses.
Conclusion
Case selection is critical for a successful outcome; regenerative medicine is not always the most appropriate therapy. Discuss treatment options with your horse’s veterinarian, taking into account the horse’s prognosis, the cost of different regenerative techniques, the rehabilitation requirements post-therapy, and your goals for the horse.
Regenerative medicine is still “young” and holds an exciting future. Horses have been one of the first animals to benefit from these techniques, and as new research is conducted and breakthroughs occur, we are likely to see even more effective healing applications for our equine friends and athletes.
Pilchuck Veterinary Hospital offers a variety of regenerative medicine techniques, including those described above: www.pilchuckvet.com.
James Bryant, DVM, Diplomate ACVS, heads Pilchuck Veterinary Hospital’s equine department, where he is a staff surgeon and lameness specialist. After receiving his veterinary degree from the University of California at Davis, College of Veterinary Medicine in 1995, Dr. Bryant completed an internship at Texas A&M University, followed by a surgical residency at the University of Florida.
Published October 2011 Issue

The Colorado Horse Source is an independently owned and operated print and online magazine for horse owners and enthusiasts of all breeds and disciplines in Colorado and surrounding area. Our contemporary editorial columns are predominantly written by experts in the region, covering the care, training, keeping and enjoyment of horses, with an eye to the specific concerns in our region.